According to recent global data, about 1 in 5 people will develop cancer during their lifetime, and approximately 1 in 9 men and 1 in 12 women die from it. These numbers show that cancer affects nearly every family, community, and healthcare system worldwide.
Despite advancements in treatment, significant gaps remain in early detection, diagnostic accuracy, and the ability to personalize care for each patient.
Artificial intelligence is beginning to bridge those gaps.
For instance, AI-powered software approved by the FDA is now helping pathologists detect prostate cancer in biopsy images.
In breast cancer screening, AI can detect tumors in mammograms with accuracy comparable to or better than that of human radiologists. Predictive models can assess cancer risk using a person’s genetics, lifestyle, and medical history.
Yet many of these innovations remain underutilized due to barriers in access and usability for clinical professionals and researchers.
This blog explores the current applications of AI in cancer research and care, the practical challenges that limit its broader use, and what needs to be done to fully realize its potential in reducing cancer mortality and improving patient outcomes.
Why Generative Models Matter in Medical Imaging?
Medical imaging plays a critical role in cancer detection, diagnosis, and treatment planning. However, the effectiveness of machine learning models in this field largely depends on the quality, diversity, and volume of imaging data available for training and validation.
Importance of Imaging Data in Cancer Research
High-quality, diverse, and annotated imaging datasets are critical for developing reliable diagnostic models in cancer research.
These datasets provide the foundation for training machine learning algorithms to detect tumors, classify cancer types, and assess disease progression. However, collecting large volumes of such data is difficult due to high costs, limited availability of rare cancer cases, and the need for expert annotations.
Addressing Data Gaps Through Augmentation
Generative models can create synthetic medical images that closely resemble real scans. This is particularly useful for augmenting datasets that lack examples of rare cancers.
By generating synthetic images for underrepresented categories, researchers can balance their datasets and reduce the risk of model bias, leading to better performance across diverse patient populations.
Enabling Privacy-Preserving Synthetic Data
Patient medical images are sensitive and subject to strict privacy regulations. Generative models allow the creation of synthetic data that replicates key clinical features without containing identifiable patient information.
This enables institutions to share and use data more freely while maintaining compliance with privacy standards.
Enhancing Model Generalizability
Diagnostic models trained on limited or homogeneous datasets often struggle to perform well in real-world clinical environments.
Generative models can simulate a wide range of image variations as differences in tumor appearance, image quality, or scanning angles, helping models become more adaptable. This improves their reliability when applied to new or unseen data.
Types of Generative Models in Oncology: Transforming Cancer Imaging and Diagnosis
As part of AI in cancer research, generative models reshape how imaging and diagnosis are approached. Generative models are a class of machine learning techniques that learn from data and then generate new data that looks similar. In cancer imaging, these models can produce synthetic scans or histology images that mimic real patient data. Below are the primary types of generative models being used:
1. GANs (Generative Adversarial Networks)
GANs consist of two neural networks, a generator and a discriminator, that are trained together. The generator creates synthetic data, such as medical images, while the discriminator evaluates whether the data is real or fake. Over time, the generator learns to produce highly realistic outputs.
- GANs can generate lifelike MRI, CT, or histopathology images. This is especially useful in cases with limited data for rare conditions.
- They expand existing datasets by creating variations of real images. This improves the performance of diagnostic models, particularly in detecting less common cancer types.
- GANs enhance the resolution of medical images, which can be critical for identifying small tumors or delicate tissue structures.
For example, GANs can improve the visibility of tumor margins in MRI scans, helping radiologists make more precise surgical decisions. They can also generate synthetic examples of rare pathologies, which aids in training robust machine learning models.
2. VAEs (Variational Autoencoders)
VAEs encode input data into a lower-dimensional space, called the latent space, and then decode it to reconstruct the original input. This structure helps identify and learn essential patterns in the data. Here is how they can be applied in cancer research:
- VAEs can detect deviations from standard patterns in medical images, making them suitable for spotting early signs of cancer or identifying unusual tumor behavior.
- By analyzing the latent space, researchers can understand relationships between different medical features, such as tumor size and shape progression.
- VAEs can reconstruct missing or damaged parts of medical images, which can be helpful in cases where data is incomplete.
For instance, VAEs have been used to detect subtle changes in cancer progression in longitudinal patient data or to fill in incomplete histopathology slides with plausible tissue structures.
3. Diffusion Models
Diffusion models gradually transform random noise into detailed images by learning how to reverse a noise-adding process. This step-by-step generation enables high control and image realism. Diffusion models generate images with finer details and better texture than GANs in many cases, making them highly suitable for medical imaging, where clarity is essential.
- Diffusion models offer more stable training and better control over the generation process, reducing artifacts sometimes seen in GAN outputs. Here is the list of applications as they are applied in cancer research:
- Diffusion models can produce high-resolution, realistic histopathology slides and ultrasound images, which support the training and validation of diagnostic models.
- Their precision makes them effective at capturing rare or complex patterns in cancer tissue that other models might miss.
Due to their superior image quality and control, diffusion models may eventually outperform GANs in medical applications, particularly where diagnostic accuracy is closely tied to visual details.
The Role of AI in Modern Cancer Research: From Clinical Data to Insights
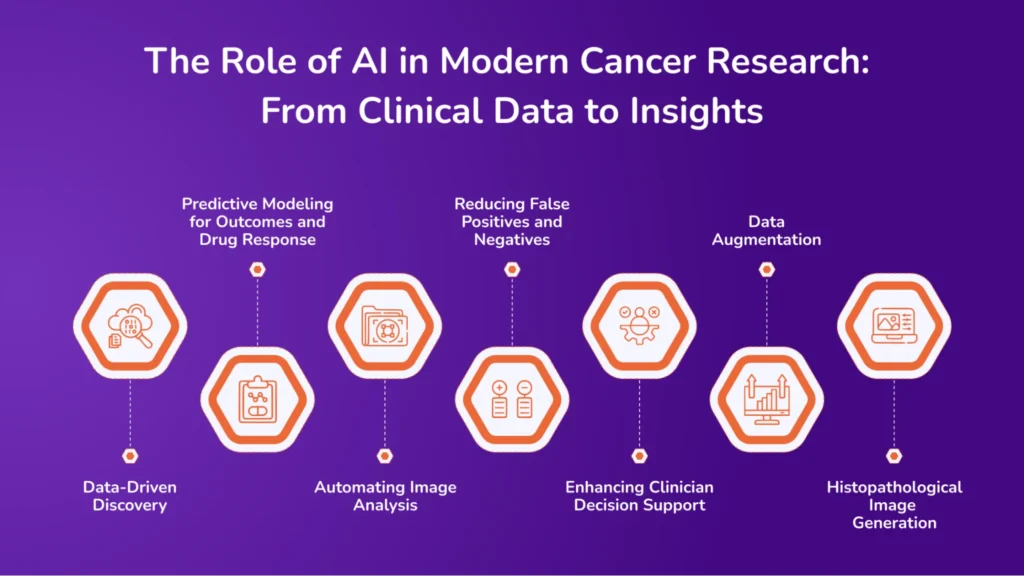
Here’s how AI in cancer research drives advancements in medical imaging and transforms the field of cancer diagnosis and analysis.
1. Data-Driven Discovery
Cancer research generates large amounts of data, from electronic health records to genetic sequencing. Manually analyzing this data is slow and prone to errors. AI tools can process vast datasets quickly and find patterns that humans might miss. AI can identify genetic mutations linked to specific cancer types and match patient profiles with suitable clinical trials.
For instance, AI tools have been used to identify links between BRCA1 gene mutations and an increased risk of breast cancer. These insights help identify individuals at risk early and guide screening or preventive measures. By analyzing both clinical history and genomic data together, AI helps researchers understand how different types of cancer behave at a molecular level.
2. Predictive Modeling for Outcomes and Drug Response
AI models can predict how a patient might respond to specific treatments. They use data from past patients, such as tumor characteristics, treatment methods, and outcomes, to make these predictions.
Applications include estimating survival rates based on treatment plans, identifying patients likely to benefit from targeted therapies, and recommending alternative treatments when standard options fail. MD Anderson Cancer Center researchers used AI to predict how lung cancer patients would respond to immunotherapy by analyzing CT scans and clinical notes. The model helped oncologists choose the most effective treatment. These models allow researchers design more effective trials and support personalized treatment planning.
3. Automating Image Analysis
AI systems can automatically analyze medical images. They detect, label, and measure tumors in scans faster than humans can. This speeds up the diagnostic process and reduces the load on radiologists and pathologists.
Typical tasks include segmenting tumors from healthy tissue, measuring tumor size and growth, and comparing changes across scans. In prostate cancer, AI tools segment tumors in MRI scans within seconds, a task that usually takes radiologists 10–20 minutes per patient.
4. Reducing False Positives and Negatives
AI can improve diagnostic accuracy. A false positive means diagnosing cancer when it’s not there, and a false negative means missing cancer when it is present. Both are harmful. AI models trained on large, diverse datasets can more reliably identify real signs of cancer and avoid unnecessary treatments for healthy patients.
For example, an AI-powered imaging system analyzed mammograms and reduced false positives by highlighting only the cases most likely to indicate cancer for further review.
5. Enhancing Clinician Decision Support
AI doesn’t replace doctors, it supports them. It provides a second opinion, highlights critical areas, and offers insights based on data patterns. This helps make faster, more informed decisions and reduces uncertainty in complex cases.
6. Data Augmentation
The large, diverse datasets are one of the most significant problems in cancer AI development. Privacy rules and the rarity of some cancers make it challenging to collect enough data to train reliable models.
Generative models generate new training examples based on real data, increasing the variety of samples, especially for underrepresented types of cancer. For example, researchers used GANs to create synthetic brain tumor MRI scans. These helped train deep learning models that performed better on small real-world datasets.
7. Histopathological Image Generation
In pathology, high-resolution images of tissue slides are essential for diagnosis and research. Generative models can create synthetic slides that replicate the structure of real tissues.
They help to create virtual slides for training AI without requiring additional lab work, fill in gaps where real slides are missing or degraded, and simulate different stages of tumor growth in tissues. For example, a study used GANs to generate images of colorectal cancer histology indistinguishable from real samples. These were used to train an AI model for tumor classification.
Critical Challenges in Using AI for Cancer Research and Medical Imaging
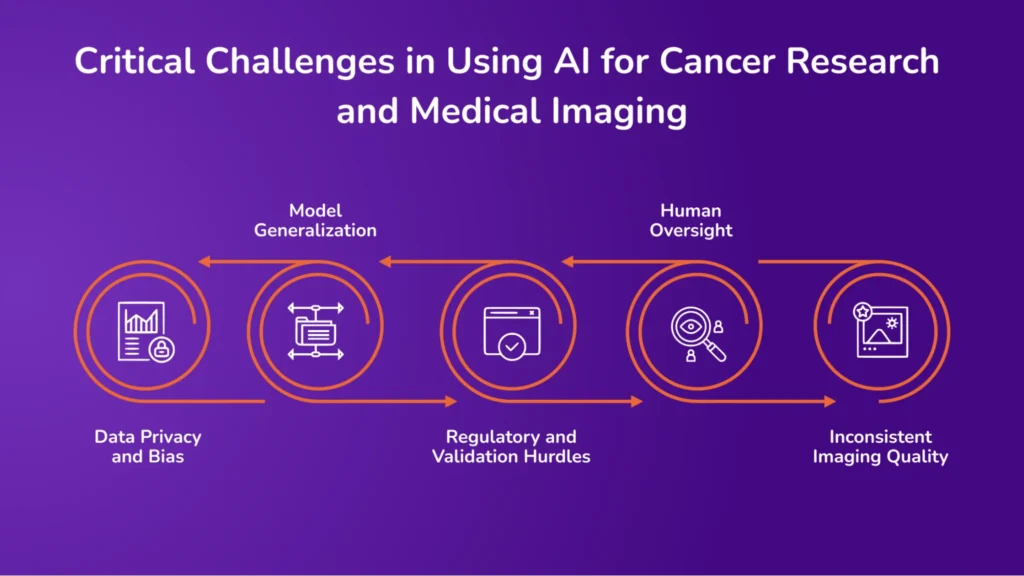
While AI in cancer research brings many benefits, it also introduces significant challenges that must be addressed. Below is the list of specific challenges in applying AI to cancer research and imaging:
1. Data Privacy and Bias
Generative AI models rely on large amounts of patient data to learn and produce accurate results. This data often includes sensitive information from medical records and diagnostic images.
Even when data is anonymized, there is always a risk of re-identification. Data breaches can expose personal health information, and sharing datasets across institutions increases exposure risks.
Synthetic data, created by generative models, can reduce dependency on real data. However, if the models are trained on biased or incomplete datasets, the synthetic output may still carry those biases or even unintentionally reflect real patient characteristics.
2. Model Generalization
AI models trained on data from one group may not perform well on data from other groups. For example, a model trained primarily on images from one ethnic group or age might not detect cancer as effectively in others.
Misdiagnosis risks increase in underrepresented populations. Healthcare inequalities can widen if models only work well for specific groups. Clinical trials and training datasets must represent many patients to ensure fairness and accuracy.
3. Regulatory and Validation Hurdles
Getting an AI tool into real-world clinical use is a complex process. Developers must prove that the tool is safe, effective, and consistent.
There are no clear regulations for AI tools in healthcare, and differences in approval processes between countries. Medical regulatory bodies, such as the FDA or EMA, have long timelines for approval. Hospitals and research institutions often hesitate to adopt these tools without formal approval, even if they show promise.
4. Human Oversight
AI is not a replacement for medical professionals. Radiologists, oncologists, and pathologists still need to review, interpret, and confirm AI-generated results.
AI can assist by highlighting areas of concern, but it may not explain how it reached its conclusion. Doctors must understand when to trust the AI and when to override it. Final diagnosis and treatment decisions must remain with trained clinicians. Without proper oversight, there is a risk of overreliance on AI, leading to mistakes, especially in complex or borderline cases.
5. Inconsistent Imaging Quality
MRI, CT, and pathology images can differ in resolution, format, and clarity, depending on the equipment or how the scan was performed. These differences make it harder to compare or analyze results consistently.
What’s Next: The Future of AI-Driven Cancer Imaging
AI in cancer imaging is advancing rapidly, and generative models are expected to play a central role in the subsequent development phase. These advancements will improve diagnostic accuracy and support more personalized and responsive cancer care.
Multi-Modal Generative Models
Future systems will likely combine multiple types of patient data, such as medical images, genomic profiles, and clinical records, into a single model.
These multi-modal generative models can produce more comprehensive insights by connecting patterns across different data types. For example, they could help link tumor appearance in imaging to specific genetic mutations, allowing for more precise diagnosis and treatment recommendations.
Personalized Treatment Planning with Synthetic Simulations
Generative models may also support personalized treatment planning by simulating how a specific patient’s cancer might respond to different therapies.
By creating synthetic scenarios based on patient data, these models can help oncologists explore potential treatment outcomes before making decisions. This approach could reduce trial and error in treatment selection, leading to more targeted care.
Integration with Real-Time Diagnostic Systems
AI-driven generative models are also being integrated into real-time diagnostic tools used in hospitals and clinics.
These systems can assist radiologists during image review by generating enhanced or alternative views, highlighting suspicious areas, or flagging anomalies in real-time. This integration can speed decision-making, reduce diagnostic errors, and provide consistent support in busy clinical environments.
The future of AI-driven cancer imaging lies in deeper data integration, personalized simulation-based planning, and seamless deployment in real-time clinical workflows. These advancements will help deliver faster, more accurate, and tailored cancer care.
Transforming Healthcare with Avahi AI: Streamlining Processes and Improving Care
The Avahi AI platform is pivotal in healthcare by providing innovative solutions that streamline medical data handling and enhance the quality of healthcare services. The platform offers several features to improve efficiency and accuracy in various aspects of healthcare, from document processing to medical transcription.
1. Smart PDF Summarizer
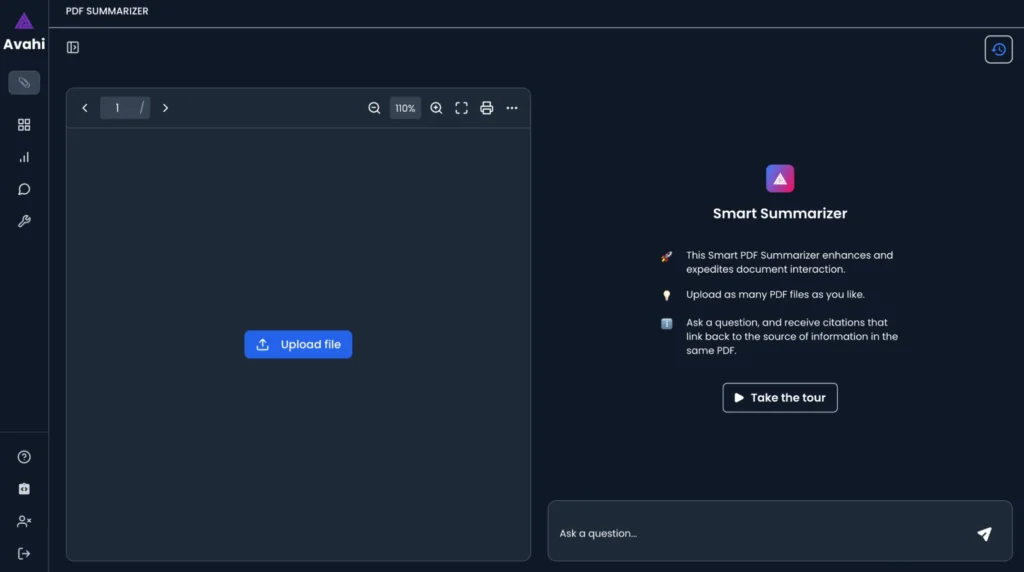
Avahi AI’s Smart PDF Summarizer makes it easier for healthcare professionals to interact with large documents, such as medical reports, research papers, and patient records. Users can generate concise summaries by uploading multiple PDF files while retaining key information.
This helps reduce the time spent reviewing lengthy documents, enabling healthcare providers to access relevant insights quickly for better decision-making. Additionally, the platform allows you to view the original text alongside the summary, providing a more comprehensive understanding of the document’s content.
Benefits:
- Time-saving: Expedites the process of reviewing and summarizing large medical documents.
- Increased accuracy: Extracts key information from complex documents, reducing human error.
- Improved decision-making: Quickly provides healthcare professionals with actionable insights from medical records and research.
2. Data Masker
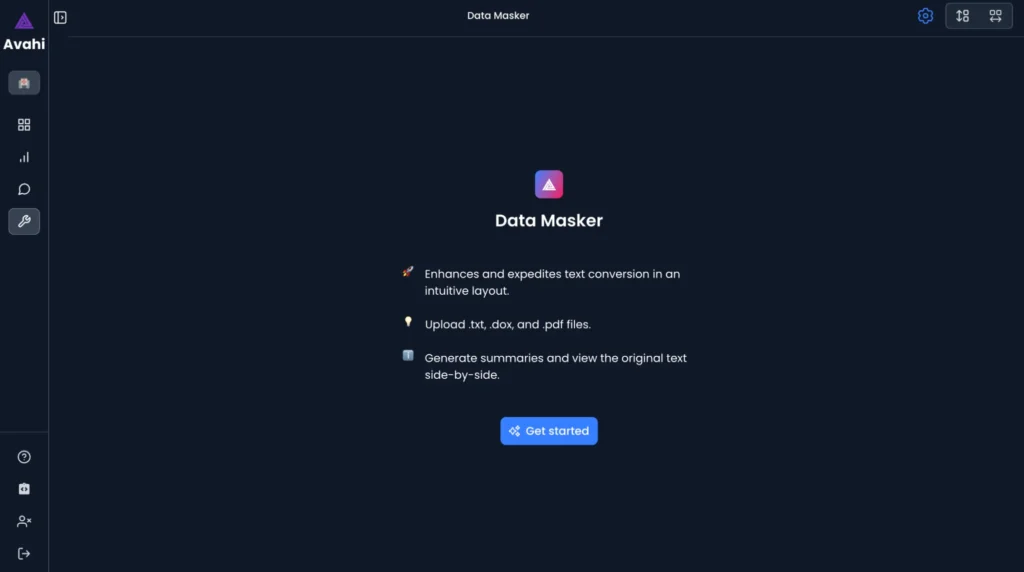
The Data Masker feature ensures data privacy and security in healthcare settings. This feature helps healthcare organizations comply with privacy regulations like HIPAA by masking sensitive patient data. This is especially beneficial when handling medical records or sharing data with third-party platforms, as it protects patient information.
Benefits:
- Enhanced privacy: Protects sensitive patient information by anonymizing data.
- Regulatory compliance: Helps healthcare organizations meet legal requirements for data protection.
- Secure data sharing: Safely shares data with researchers or other healthcare providers without compromising patient confidentiality.
3. Medical Scribing
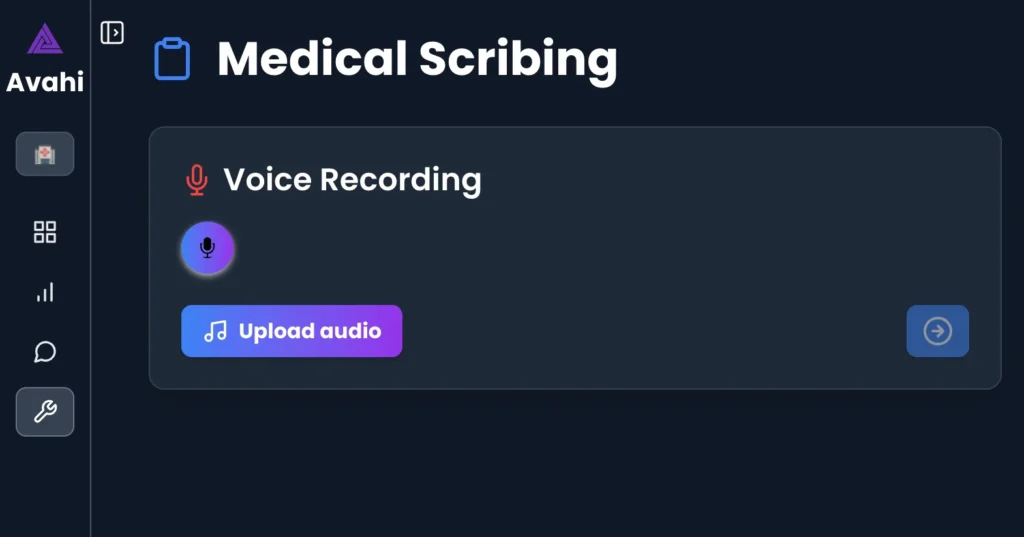
Avahi AI’s voice recording and medical scribing features support healthcare professionals by transcribing verbal notes into written text. This is particularly useful for physicians and medical staff who need to document patient interactions but don’t have much time to do so. By using voice recordings, healthcare providers can capture important patient information quickly and accurately without having to type out notes manually.
Benefits:
- Efficiency: Speeds up the documentation process by converting voice to text.
- Accuracy: Reduces the risk of errors that can occur when typing manually.
- Convenience: Allows healthcare providers to focus more on patient care while letting the AI platform handle the transcription.
Discover Avahi’s AI Platform in Action
At Avahi, we empower businesses to deploy advanced Generative AI that streamlines operations, enhances decision-making, and accelerates innovation—all with zero complexity.
As your trusted AWS Cloud Consulting Partner, we empower organizations to harness AI’s full potential while ensuring security, scalability, and compliance with industry-leading cloud solutions.
Our AI Solutions Include
- AI Adoption & Integration – Utilize Amazon Bedrock and GenAI to enhance automation and decision-making.
- Custom AI Development – Build intelligent applications tailored to your business needs.
- AI Model Optimization – Seamlessly switch between AI models with automated cost, accuracy, and performance comparisons.
- AI Automation – Automate repetitive tasks and free up time for strategic growth.
- Advanced Security & AI Governance – Ensure compliance, fraud detection, and secure model deployment.
Want to unlock the power of AI with enterprise-grade security and efficiency?
Get Started with Avahi’s AI Platform!